Beyond Birth: Maternal health realities before and after the delivery room
In 2020, Delegate Marcia Price (95th District) boldly introduced a resolution in the House of Delegates to establish the observance of July as Maternal Health Awareness Month in Virginia. Responding to the alarming number of cases of preventable pregnancy-associated deaths of Black women in the Hampton Roads region—the highest in the Commonwealth—her voice elevated the maternal health needs that exist outside the delivery room, widening the scope of care and concern beyond the birthing moment.
“What we are trying to use July to do is raise awareness about the things that have been proven to better the health outcomes of both mother and baby,” she explained to the House Committee on Rules before its vote on the resolution on January 24, 2020. She continued her comments in response to a concern of the resolution’s mention of the negative impacts of structural racism on the health outcomes for Black women, highlighting a 2016 study conducted by the University of Virginia no less. “While I would hope that structural racism and its effects would have been in the past, it is still happening in our present. We are trying to fund initiatives that would counteract this with training.”
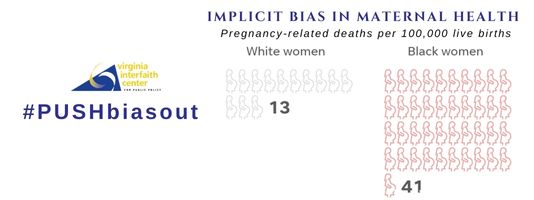
We agree. And that is why we are still pushing for an implicit bias training criterion for licensure of all health care professionals who have direct contact with patients. Two years later, and the latest data on maternal mortality for Black women in the U.S. regrettably upholds Del. Price’s position before the House Committee.
According to a study released this past April by the Commonwealth Fund, the U.S. had the highest rates of women dying from avoidable causes in pregnancy-related complications, with 198 per 100,000 live births in 2020. On the opposite end of the spectrum, in 2019 (the latest data available there), Norway had zero maternal deaths. You read that right. Zero.
The study also found that the U.S. maternal mortality rate is not just the highest among the other 10 high-income countries in the study, it is more than triple the rate of the other countries, with 23.8 deaths per 100,000 live births. Here is the alarm bell that continues to ring louder in the data: the Black maternal mortality in the U.S. is 55.3 deaths per 100,000 live births.
“Pregnancy shouldn’t kill people—in fact in other rich countries, it very rarely does,” said Amanda Stevenson, assistant professor of sociology at the University of Colorado and one of the researchers at its Institute of Behavioral Science who this month released a study on the current realities of maternal mortality.
In recognition of Virginia’s Maternal Health Awareness Month, VICPP has launched a monthlong social media focus, #BeyondBirth, as part of our #PUSHbiasout campaign. We will share women’s stories, research from medical experts, quotes from birth equity advocates who participated in our PSA series, reflections on the sacred texts that comprise “What Faiths Say About Maternal Health,” and video clips from legislative testimony, and remarks by organizational leaders. We invite you to read and share our daily posts to raise awareness and understanding about the stark maternal mortality realities, efforts to mitigate the prevalent harm, and proven interventions to improve the health outcomes of Black birthing people.
Tune into our discussion next Monday, July 11 (World Population Day), with the Black Women’s Health Imperative Director of Maternal and Child Health Dr. Kanika Harris immediately following our screening of the documentary film about their work, “In Sickness and In Health: Overcoming Bias.” CLICK HERE TO REGISTER
